Introduction to IgG and Its Emerging Role in Metabolic Dysfunction
Immunoglobulin G (IgG) has long been recognized as a key player in the immune system, primarily circulating in the bloodstream to combat pathogens. However, recent research has uncovered a surprising role for IgG in metabolic dysfunction, particularly in the contexts of obesity and aging. This article delves into the mechanisms by which IgG contributes to metabolic issues and explores potential therapeutic avenues.
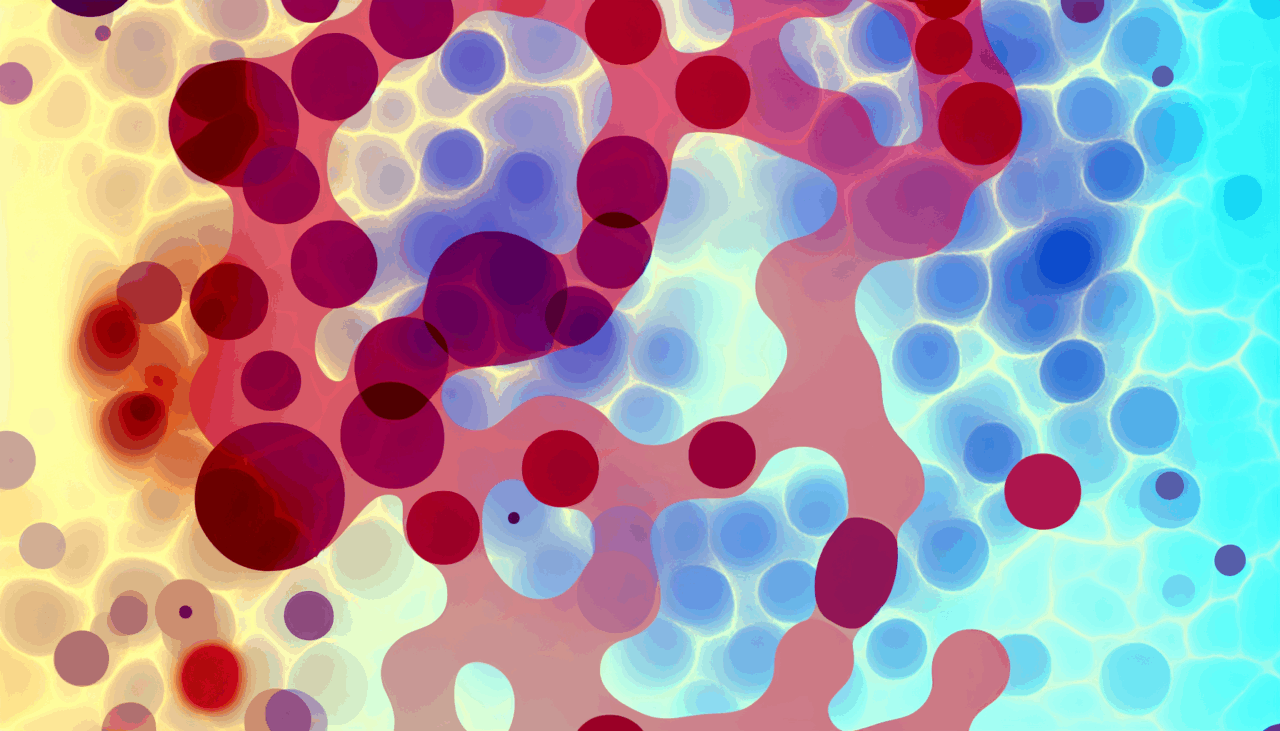
IgG Accumulation in Adipose Tissue
Traditionally viewed as a circulating immune effector, IgG has been found to accumulate in adipose tissue at levels up to 16 times higher than in plasma. This accumulation is mediated by the neonatal Fc receptor (FcRn), which facilitates IgG uptake into adipose cells. Interestingly, IgG competes with insulin for receptor binding through interactions in the Fc-CH3 domain, highlighting its significant role in metabolic processes.
Inflammatory Responses and Glycosylation Patterns
IgG’s impact on metabolic dysfunction is closely tied to its glycosylation patterns. Sialylated IgG, often referred to as control IgG, engages anti-inflammatory pathways via receptors such as DC-SIGN and CD22. In contrast, hyposialylated IgG, which is associated with disease, activates endothelial FcγRIIB receptors. This activation impairs insulin transcytosis and promotes vascular insulin resistance, offering insights into why traditional anti-inflammatory treatments may fall short in addressing metabolic diseases.
Progression of IgG-Mediated Effects
The timeline of IgG’s effects on metabolism unfolds in stages. Initially, there is acute inflammation lasting weeks, followed by subacute deposition and interference with insulin over months. Eventually, chronic fibrosis can develop over years. These stages underscore the complex nature of IgG’s role in metabolic dysfunction and the need for targeted interventions.
Therapeutic Implications and Biomarker Potential
Research suggests that antagonists of FcRn can reverse insulin resistance, while restoring IgG sialylation using sialic acid precursors can improve metabolic function without depleting antibodies. These findings open up new possibilities for biomarkers and therapeutic targets in the treatment of metabolic diseases. Glycosylation profiling, for instance, can distinguish between individuals who are insulin-sensitive and those who are resistant, even if they have similar body mass indices. This supports the development of precision medicine approaches tailored to individual metabolic profiles.
Reframing Metabolic Disease Pathogenesis
The discovery of IgG’s role in metabolic dysfunction represents a paradigm shift from traditional cell-centric models to antibody-mediated models. This new understanding reframes the pathogenesis of metabolic diseases and suggests novel treatment strategies that could significantly impact patient outcomes.
Conclusion
The intersection of IgG dysfunction with obesity, aging, and metabolic disease offers a rich area for further research and therapeutic development. By focusing on the unique role of IgG in these processes, scientists and clinicians can develop more effective strategies to combat metabolic dysfunction and improve health outcomes.
🔗 **Fuente:** https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1661391/full